As the year comes to a close, people are starting to puke. The notorious stomach bug known as norovirus is starting its annual rampage, which will last from late fall through winter. A couple years ago, in the midst of another norovirus season, I wrote about the virus’s spectacular biology on the Loom. Noroviruses (unlike the Ebola virus) are extraordinarily rugged, able to waft through the air and survive for days on surfaces where it can cause a new infection. In a scientific review, one CDC scientist went so far as to declare, “noroviruses are perhaps the perfect human pathogen.”
This exquisite potency makes noroviruses a massive burden on our collective health. According to the latest estimates, noroviruses infect about 20 million Americans every year, and many more worldwide. But despite the scale of their threat, the fight against noroviruses has been slow. That’s because no one has been able to rear human noroviruses in the lab. To run experiments to see how noroviruses makes us sick, to develop vaccines, and to test out antiviral drugs, scientists desperately want a recipe for brewing up batches of noroviruses.
The inability to raise noroviruses stems, in turn, from our ignorance about some of the most important aspects of their biology. Scientists know that the virus attacks the gut, but they haven’t known for sure which kind of cell it attacks, or how it does so. They know that different noroviruses are more dangerous to people with different blood types–despite the fact that norovirus does not cause blood disease.
But now a team of scientists led by Stephanie Karst of the University of Florida may have cut through a lot of these mysteries. Karst and her colleagues have figured out how noroviruses get into our cells. And it turns out that some of our harmless gut bacteria are helping the viruses get there.
For years, scientists had assumed that noroviruses infected the cells that make up the inner lining of the intestines. After all, those cells (called epithelial cells) were the first ones that the viruses would encounter when they arrived in the gut.
If noroviruses infected epithelial cells, scientists could also explain the puzzling link to blood types. Our blood types are determined by the type of carbohydrates that festoon our red blood cells. But our gut epithelial cells also put the same carbohydrates on their surface too. Noriviruses can bind to these carbohydrates (known officially as human blood group antigens, or HBGAs).
Add up all the evidence, and you got a pretty straightforward scenario: noroviruses arrive in the gut, latch onto the HBGAs on the epithelial cells, invade those cells, and voila, a weekend of vomiting and diarrhea.
As sensible as that scenario sounded, though, there was one big problem: when scientists would run experiments, the viruses didn’t show any interest in infecting epithelial cells. Nor did the viruses seem to stay around on the surface of the intestines. Karst and her colleagues infected mice with a mouse version of norovirus, they found that it somehow burrowed deep inside the intestinal lining.
Buried deep in the lining of our gut, there are pouches of immune cells that protect us from intestinal infections. As food slides down through the intestines, the epithelial cells pick out suspicious-looking proteins and deliver them into those pouches. Cells known as B cells can then make antibodies that attack dangerous pathogens.
The deep dive that the noroviruses were taking raised the possibility that they were infecting B cells in the gut. Karst and her colleagues got even more interested in B cells when they ran another experiment on mice. The scientists were hoping to better understand how a norovirus infection may protect a mouse for future infections. As part of their experiment, they reared mice that couldn’t make B cells.
You might expect that the mice would become less able to withstand norovirus infections, since they couldn’t make antibodies. But the opposite was true: without B cells, the mice became more resistant.
Pondering all these pieces of evidence, Karst and her colleagues suspected that maybe B cells–not epithelial cells–really were the target of noroviruses.
The scientists tested out the idea on mouse noroviruses. When they mixed mouse noroviruses in a dish with mouse B cells, the viruses could indeed invade the cells, as the scientists predicted. But when they tried to infect epithelial cells, on the other hand, the viruses failed to invade.
The scientists couldn’t be sure that what was true for mice was true for humans. But testing their idea on human noroviruses would be a lot harder, since Karst and her colleagues didn’t have an endless supply of pure noroviruses.
Instead, the scientists had to collect stool samples from sick patients. They diluted the virus-laden stool and mixed it with human B cells. Just as they had hoped, the viruses infected the B cells.
There was, however, a fascinating catch. If the scientists put the stool through very fine filters–fine enough to exclude bacteria–the noroviruses could no longer infect the B cells.
This failure suggested that resident gut bacteria–or at least one species of bacteria–were helping the noroviruses.
It would have been absurd for Karst and her colleagues to test out every species of gut bacteria to see which one was aiding the noroviruses. Our guts contains many hundreds of species. Fortunately, previous research by other scientists allowed Karst and her colleagues to avoid this brute-force approach.
It turns out that blood type cells and epithelial cells are not the only cells to produce blood-type molecules. Certain species of bacteria have HBGAs, too. It’s not clear why they have the same molecules as we do. But whatever the reason, noroviruses can grab onto bacterial HBGAs as well as they can onto our own.
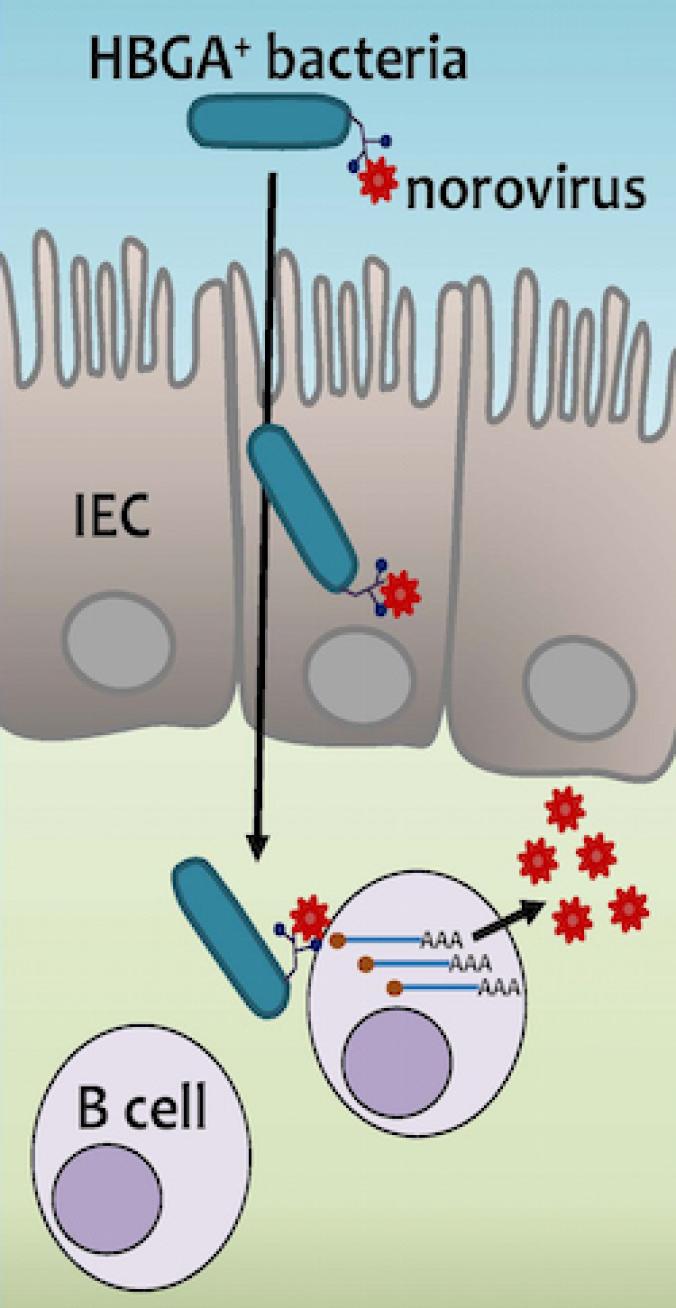
Karst and her colleagues picked out one of the species that other scientists had shown could bind noroviruses. It’s a common kind of bacteria called Enterobacter cloacae. The scientists added Enterobacter cloacae to filtered stool samples that contained human noroviruses. And then they combined this mixture with human B cells. Now they could get human noroviruses to infect B cells.
This experiment doesn’t reveal precisely how Enterobacter cloacae help noroviruses get into B cells. It’s possible that the bacteria ferry them into the hidden pouches where B cells lurk. It’s also possible that when the viruses latch onto the bacteria, the connection triggers a change in their surface molecules, making it possible for them to infect the cells. Karst hopes to get some answers with more research.
But this new results may offer an explanation for why people’s blood types make them more or less vulnerable to noroviruses. Let’s say you’re type B. Your immune system learns to recognize type B HBGAs as harmless, because they’re part of your own body. It’s possible that if you’re colonized by bacteria that have type B HBGAs, too, your body will tolerate them as well.
But if you get infected with bacteria that carry type A HBGAs, your immune system may make antibodies and attack them as foreign. That’s the likely reason that getting a tranfusion with the wrong blood type can be so dangerous. If you are Type B, for example, you have lots of antibodies to Type A HBGAs. So your body will attack Type A blood as foreign.
The new study from Karst and her colleagues may also explain why noroviruses seem to care about your blood type. Your blood type may determine the kinds of bacteria that can survive in the gut–and thus the kinds of bacteria that noroviruses can latch onto and use to get into B cells.
It would be great to say that this discovery immediately points to a sure-fire cure for the noroviruses blues. It doesn’t, alas. Karst and her colleagues were able to block norovirus infection in mice by using antibiotics to wipe out their gut bacteria. Without bacteria to help, the virus couldn’t get into B cells. But that’s the sort of cure that’s worse than the disease. The microbiome performs lots of important tasks, including helping with digestion and creating a kind of ecological barrier that prevents nasty pathogens from invading. Take it away, and you could get very sick–much sicker than you’d be with a norovirus infection.
Nevertheless, this discovery is still important, because it explains why previous attempts to raise noroviruses have failed. The viruses were provided with the wrong target and didn’t get the help they needed to hit it. Now, Karst hopes, she and her colleagues can finally develop a recipe to brew up lots and lots of human noroviruses for research on vaccines and antivirals.
And that’s the only sense in which the phrase “lots of lots of noroviruses” can make us happy.